My mother started Passover cleaning in February. Yes
— February. So when I came back to my parents’ home, I helped sort
through a few old childhood boxes. In one of them, tucked between my diaries
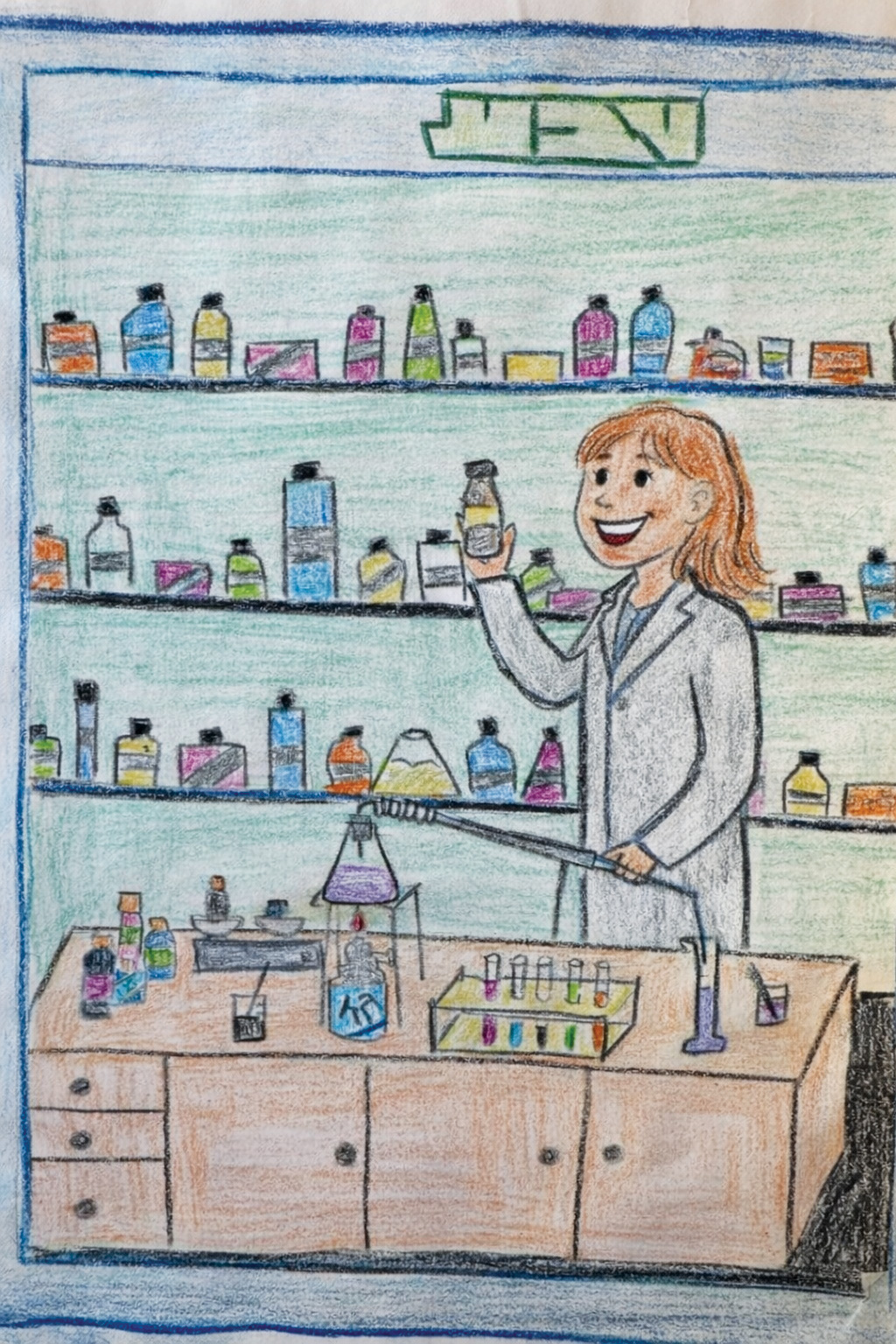
and school notebooks, I found a drawing I had made at the age of ten. My
third-grade teacher in Tel Aviv had given us an assignment: “Draw how you
see yourself in the future.”
In my picture, I had carefully sketched TEVA’s green,
italicized, four-letter logo in the top right corner. Behind it were shelves
upon shelves of neatly arranged boxes and bottles — my very organized, serious
childhood vision of a pharmacy. And there I was: an older version of myself,
maybe in my thirties, standing behind a counter with a warm, welcoming smile,
holding a paper prescription in one hand and a pill bottle in the other,
proudly dressed in a white coat.
 I don’t know where my interest in chemistry and medications
came from, but genetics may have played a role: my great-grandfather was a
well-known chemistry professor in Dushanbe during the Soviet era, and relatives
on my grandmother’s side worked in forensic science in Dushanbe and
pharmaceutical manufacturing in Israel.
I don’t know where my interest in chemistry and medications
came from, but genetics may have played a role: my great-grandfather was a
well-known chemistry professor in Dushanbe during the Soviet era, and relatives
on my grandmother’s side worked in forensic science in Dushanbe and
pharmaceutical manufacturing in Israel.
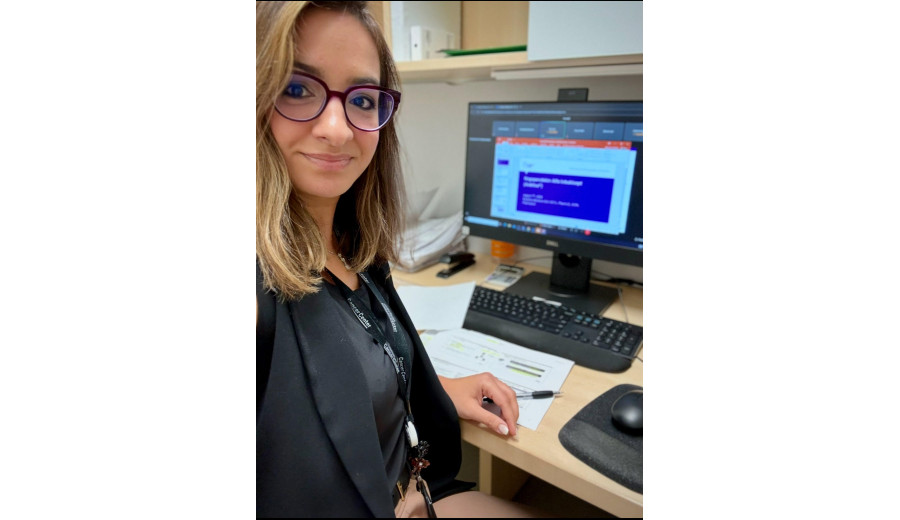
Fast forward twenty years. At 35, I am — Baruch HaShem
— indeed a pharmacist. I still wear a white coat (at least some days), still
carry that same smile I drew all those years ago, and my work still revolves
around medications. I speak daily with physicians, nurses, and fellow
pharmacists, and the responsibility feels just as meaningful as my ten-year-old
self imagined.
But here’s the twist I could never have predicted: Instead
of being surrounded by shelves of capsules, creams, and syrups, I now work
among computers, automation, digital platforms — and yes, artificial
intelligence. Nice to meet you, my name is Rozalina, and I am an Oncology
and Hematology Pharmacy Informatics Specialist at a large, 12-location
cancer center network in the New York Tri-State area.
Oncology is a unique and highly specialized corner of pharmacy. In fact, most pharmacy schools dedicate only a lecture or two to cancer medications — not because they’re unimportant, but because the field is expanding at lightning speed. New treatments are researched, FDA-approved, and brought to market almost every month.

When I first walked into an outpatient infusion center as a
pharmacy intern, it felt like landing on another planet. The medications
weren’t the familiar names I’d learned in school. Instead, they sounded like
complex, almost musical strings of syllables: Ado-trastuzumab emtansine.
Inotuzumab ozogamicin. Mirvetuximab soravtansine. And then there were
investigational drugs with no names at all — just letters and numbers that
looked more like license plates than medications.
As a chemistry major stepping into this wonderland of
molecules, I was completely fascinated. During any quiet moments between
compounding IV medications and organizing medication shelves, I devoured
package inserts — those long, white papers with impossibly tiny font tucked
into every medication box. I wanted to know everything: What does this drug
treat? How does it work at the molecular level? Why does it cause certain side
effects? How do we monitor patients to make sure these powerful, hazardous
medications help more than they harm? That curiosity pulled me into oncology
pharmacy.
After graduating from pharmacy school, I spent about five
years working as an oncology pharmacist in busy infusion centers, where more
than 150 children and adults received chemotherapy each day. Some patients came
in for a single injection; others received twelve different medications in one
visit.
My role was multifaceted. I verified every medication order
by reviewing treatment plans and lab results, ensuring doses were safe and
appropriate. I compounded chemotherapy looking like an astronaut- wearing
layers of protective gowns, masks, hair covers, and booties. I partnered
closely with physicians and nurses to adjust treatments in real time. Behind
the scenes, I also managed inventory systems, tracked controlled substances,
monitored medication waste, and prepared clinical and financial review
presentations for leadership meetings on newly approved cancer drugs.
So if you’ve ever waited for an infusion and wondered why it
takes time — there is always a pharmacist in the background, carefully
compounding medications and triple-checking every detail to make sure your
treatment is safe and tailored specifically for you.
Eventually, I felt the pull to make an impact beyond one
patient at a time. I could see the oncology “machine” growing busier — higher
patient volumes, increasingly complex therapies, and more data than any human
could reasonably process alone. That’s when I realized that pharmacy
informatics — the intersection of medication expertise, technology, and
workflow design — could help strengthen the system, reduce errors, and improve
care for patients on a much larger scale.
 Today, as an oncology informatics pharmacist, I collaborate
with physicians, nursing and pharmacy leadership, safety teams, laboratory
services, and revenue teams. Together, we design safer workflows, build
clinical alerts that stop potential mistakes before they reach a patient, and
optimize robotic systems that store, package, and even compound medications.
This work often happens behind the scenes, but its impact is felt everywhere.
The systems we build now support dozens of cancer centers across the Tri-State
area, caring for hundreds of patients every single day.
Today, as an oncology informatics pharmacist, I collaborate
with physicians, nursing and pharmacy leadership, safety teams, laboratory
services, and revenue teams. Together, we design safer workflows, build
clinical alerts that stop potential mistakes before they reach a patient, and
optimize robotic systems that store, package, and even compound medications.
This work often happens behind the scenes, but its impact is felt everywhere.
The systems we build now support dozens of cancer centers across the Tri-State
area, caring for hundreds of patients every single day.
And yes — I now help develop AI-based pharmacy
verification tools.
 Recently, I led a continuing education presentation for
pharmacists, technicians, students, and residents, including hospital pharmacy
leaders, managers, and directors. The focus was the future of our profession —
and how we can responsibly integrate artificial intelligence (AI) into oncology
pharmacy practice. AI offers exciting opportunities to enhance efficiency and
clinical care, but its success depends on thoughtful evaluation, new
technological and data-literacy skills, and evolving regulatory frameworks.
Preparing students and supporting practicing pharmacists and technicians will
be essential as AI becomes part of everyday practice.
Recently, I led a continuing education presentation for
pharmacists, technicians, students, and residents, including hospital pharmacy
leaders, managers, and directors. The focus was the future of our profession —
and how we can responsibly integrate artificial intelligence (AI) into oncology
pharmacy practice. AI offers exciting opportunities to enhance efficiency and
clinical care, but its success depends on thoughtful evaluation, new
technological and data-literacy skills, and evolving regulatory frameworks.
Preparing students and supporting practicing pharmacists and technicians will
be essential as AI becomes part of everyday practice.
The reason I’m sharing this story is simple. I want young
students — especially those just beginning to imagine their future careers — to
know that pharmacy offers far more paths than the community counter most people
are familiar with.
Community pharmacy is a vital and incredibly demanding
profession. It requires sharp attention to detail, constant multitasking,
leadership, and emotional resilience. Pharmacists are often the last stop for
patients who are tired, sick, overwhelmed, and searching for relief. I know
this firsthand. I worked in community settings as an intern, and I have deep
respect for the pharmacists who show up and do this work every day.
 But today, pharmacy is expanding in every direction. When I
graduated, the “big three” career paths were community, hospital, or industry.
Now, the landscape includes informatics, population health, specialty pharmacy,
regulatory science, oncology operations, artificial intelligence development,
pharmacogenomics— and many roles that didn’t even exist a decade ago. Our
profession is growing, and we’re advocating more than ever for pharmacists to
practice at the top of their license, with broader clinical authority and
deeper involvement in patient care.
But today, pharmacy is expanding in every direction. When I
graduated, the “big three” career paths were community, hospital, or industry.
Now, the landscape includes informatics, population health, specialty pharmacy,
regulatory science, oncology operations, artificial intelligence development,
pharmacogenomics— and many roles that didn’t even exist a decade ago. Our
profession is growing, and we’re advocating more than ever for pharmacists to
practice at the top of their license, with broader clinical authority and
deeper involvement in patient care.
So if you’re a student reading this — or a parent, mentor,
or teacher of one — know this: pharmacy is not a single road. It’s a vibrant
map with many routes, some well-traveled and others waiting to be drawn. The
future starts with a blank page, a big dream, and the courage to draw it — and
more often than not, that first sketch is more accurate than you ever
imagined.
Rozalina Abramov, Doctor of Pharmacy